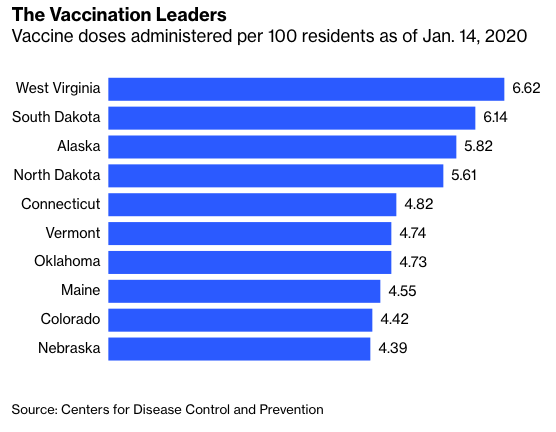
Some U.S. states are rolling out Covid-19 vaccination campaigns much faster than others. Why is that?
The Department of Health and Human Services allocates vaccines to states proportionately on the basis of their 18-and-older populations — so unlike with countries, where availability of vaccine so far seems to be the biggest determinant of vaccination rates, the states that are getting shots into arms quicker might actually have some useful lessons for others to emulate.
Here are the top 10 if you divide by each state’s number of health-care workers and residents 65 and older.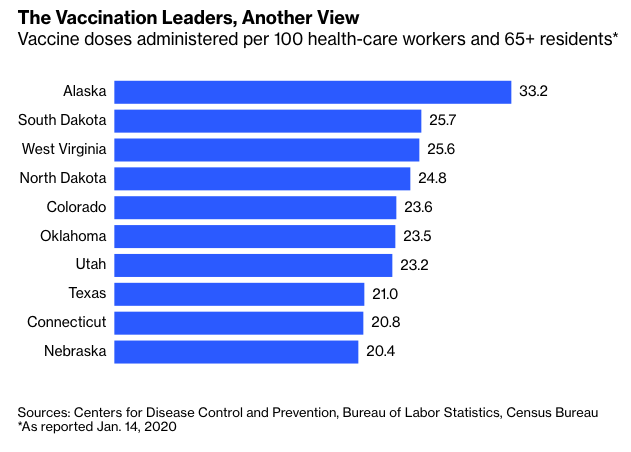
West Virginia, South Dakota, North Dakota and Alaska are the clear standouts, taking the top four spots on both lists. Remember, Alaska has twice as many vaccine doses on hand per capita as other states, so it’s probably worth waiting till the end of the month when its supply is closer to parity before declaring it to have discovered some sort of vaccination special sauce. It’s worth noting that at the moment, people in Alaska don’t seem at all impressed with the state’s rollout.
With West Virginia, on the other hand, it’s pretty clear what’s behind its high vaccination rate. Instead of waiting for the federal Pharmacy Partnership for Long-Term Care, in which CVS Inc., Walgreens Boots Alliance Inc. and several regional pharmacy chains manage vaccinations at nursing homes and other long-term care facilities, the state organized its own long-term-care vaccination program via independent pharmacies and got it started before the federal one. “West Virginia is a small, rural state, and we don’t have a city with more than 50,000 people,” the head of the state’s Independent Pharmacy Association told the Washington Examiner. “But what we do have is many small communities with small pharmacies that are trusted in those communities.”
The CVS-Walgreens program is up and running now, but still a bit behind. According to Thursday’s CDC data, it had administered just 26% of the vaccine doses it had received, while 38% of the doses available outside the program had been administered. The companies say they’ll be done with the first round of vaccinations in nursing homes and assisted-living facilities nationwide by Jan. 25, so it’s possible this disparity will soon disappear and West Virginia’s outperformance will become a thing of the past. But it’s also conceivable that the take-charge-of-its-own-destiny approach that led to the state’s nursing-home success will continue to pay dividends as other groups are vaccinated.
Similar take-charge attitudes seem to have played a role in the Dakotas, albeit in different ways. My initial suspicion was that they too had bypassed the CVS/Walgreens long-term care program but just been quieter about it. When I asked the people at South Dakota’s health department, though, they said 63% of the state’s long-term care facilities had participated in the federal program. I asked the North Dakotans later and haven’t heard back yet, and I don’t even know if 63% is high or low relative to other states (more research is needed), but the fact that a majority participated does seem to indicate that this probably isn’t the main explanation for the state’s success.
One thing that does appear to be unique about South Dakota’s vaccination effort is the extent to which it has been outsourced to the state’s three big hospital systems, Sanford Health and Avera Health of Sioux Falls and Monument Health of Rapid City, which together with a couple of smaller health-care providers have divvied up all the state’s counties and taken responsibility for vaccine provision in every one. It seemed telling that, when Sioux Falls Mayor Paul Ten Haken held his regular Covid briefing early this week, he quickly handed the microphone over to doctors from Sanford and Avera, saying he’d “leave it to the docs to talk about vaccines.” Prominent Johns Hopkins University surgeon and medical researcher Marty Makary argued this week that “hospitals should stop giving excuses and start showing some leadership” on Covid vaccination efforts rather than waiting for orders from state public health officials. In South Dakota, that was the plan from the beginning.
In North Dakota the state health department has been more visible, after participating with three other states (California, Florida and Minnesota) in a CDC Covid-vaccine-planning pilot program this fall. But Sanford Health, the leading player in its two most-populous metropolitan areas, Fargo and Bismarck, as well as some smaller communities, also seems to have played a crucial role by using its network of 180 couriers in Dodge Caravans to begin delivering the BioNTech-Pfizer vaccine to rural medical outposts in the Dakotas and Minnesota even as other rural areas around the country waited on the easier-to-store Moderna vaccine.
In general, states with a high percentage of the population in rural areas seem overrepresented on both charts above, perhaps an indication that having lots of people far from hospitals forces a more pro-active approach. States with small populations are overrepresented too, almost certainly an indication that it can be easier to get stuff done when there are fewer people and organizations to consult and coordinate.
One thing that I expected to see in the top-performing states — but didn’t — was more-relaxed rules about who could get the vaccines. New York City Mayor Bill de Blasio complained loudly last week that the state’s strict eligibility rules were holding back vaccination, and after they were relaxed this Monday there were complaints that the sign-up system was incomprehensibly complex. But New York’s vaccination rates put it in the middle of the pack among states, while top performers West Virginia and the Dakotas don’t seem to have been any less strict about eligibility in the first wave of vaccinations. Meanwhile, the state with the lowest vaccination rate by both the measures used above, Alabama, has been giving counties flexibility to ease eligibility rules if they have excess vaccine. An ability and a desire to push vaccines out quickly to those eligible for them seems to have been more important, in the early weeks at least, than the eligibility rules themselves.
On the theory that all happy families are alike while each unhappy family is unhappy in its own way, I didn’t spend much time looking at the vaccine laggards. Also it’s early yet, and it may turn out that some of the differences we’re looking at now have more to do with vaccination reporting systems than actual vaccinations. The Covid-19 pandemic has repeatedly made fools of those declaring victory prematurely. Still, states are inevitably learning from their own vaccination mistakes. Might as well try to learn from others’ successes too.
Justin Fox is a Bloomberg Opinion columnist covering business. He was the editorial director of Harvard Business Review and wrote for Time, Fortune and American Banker. He is the author of The Myth of the Rational Market.