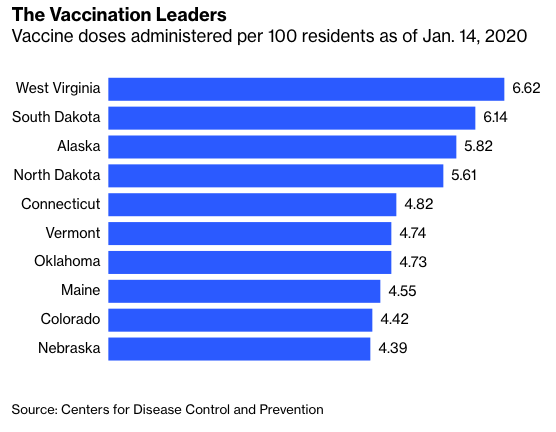
Some U.S. states are rolling out Covid-19 vaccination campaigns much faster than others. Why is that?
The Department of Health and Human Services allocates vaccines to states proportionately on the basis of their 18-and-older populations — so unlike with countries, where availability of vaccine so far seems to be the biggest determinant of vaccination rates, the states that are getting shots into arms quicker might actually have some useful lessons for others to emulate.
Here are the top 10 if you divide by each state’s number of health-care workers and residents 65 and older.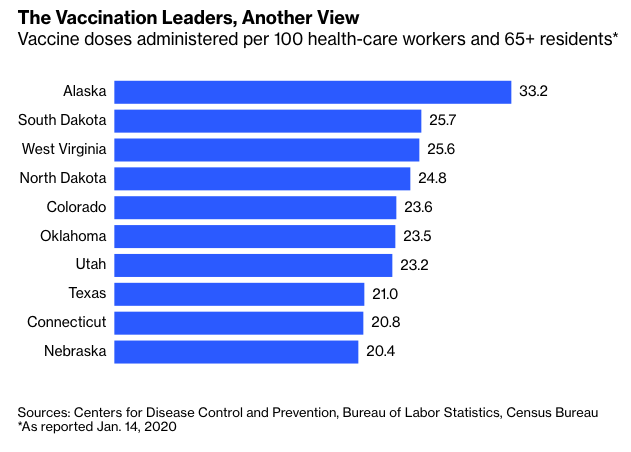
West Virginia, South Dakota, North Dakota and Alaska are the clear standouts, taking the top four spots on both lists. Remember, Alaska has twice as many vaccine doses on hand per capita as other states, so it’s probably worth waiting till the end of the month when its supply is closer to parity before declaring it to have discovered some sort of vaccination special sauce. It’s worth noting that at the moment, people in Alaska don’t seem at all impressed with the state’s rollout.
With West Virginia, on the other hand, it’s pretty clear what’s behind its high vaccination rate. Instead of waiting for the federal Pharmacy Partnership for Long-Term Care, in which CVS Inc., Walgreens Boots Alliance Inc. and several regional pharmacy chains manage vaccinations at nursing homes and other long-term care facilities, the state organized its own long-term-care vaccination program via independent pharmacies and got it started before the federal one. “West Virginia is a small, rural state, and we don’t have a city with more than 50,000 people,” the head of the state’s Independent Pharmacy Association told the Washington Examiner. “But what we do have is many small communities with small pharmacies that are trusted in those communities.”
The CVS-Walgreens program is up and running now, but still a bit behind. According to Thursday’s CDC data, it had administered just 26% of the vaccine doses it had received, while 38% of the doses available outside the program had been administered. The companies say they’ll be done with the first round of vaccinations in nursing homes and assisted-living facilities nationwide by Jan. 25, so it’s possible this disparity will soon disappear and West Virginia’s outperformance will become a thing of the past. But it’s also conceivable that the take-charge-of-its-own-destiny approach that led to the state’s nursing-home success will continue to pay dividends as other groups are vaccinated.
Similar take-charge attitudes seem to have played a role in the Dakotas, albeit in different ways. My initial suspicion was that they too had bypassed the CVS/Walgreens long-term care program but just been quieter about it. When I asked the people at South Dakota’s health department, though, they said 63% of the state’s long-term care facilities had participated in the federal program. I asked the North Dakotans later and haven’t heard back yet, and I don’t even know if 63% is high or low relative to other states (more research is needed), but the fact that a majority participated does seem to indicate that this probably isn’t the main explanation for the state’s success.








